The Power of Combined Treatment: How to Integrate Antidepressants into Trauma-Based Therapy
Let’s be real- dealing with trauma, especially the enduring response to it in our brain and body, sucks.
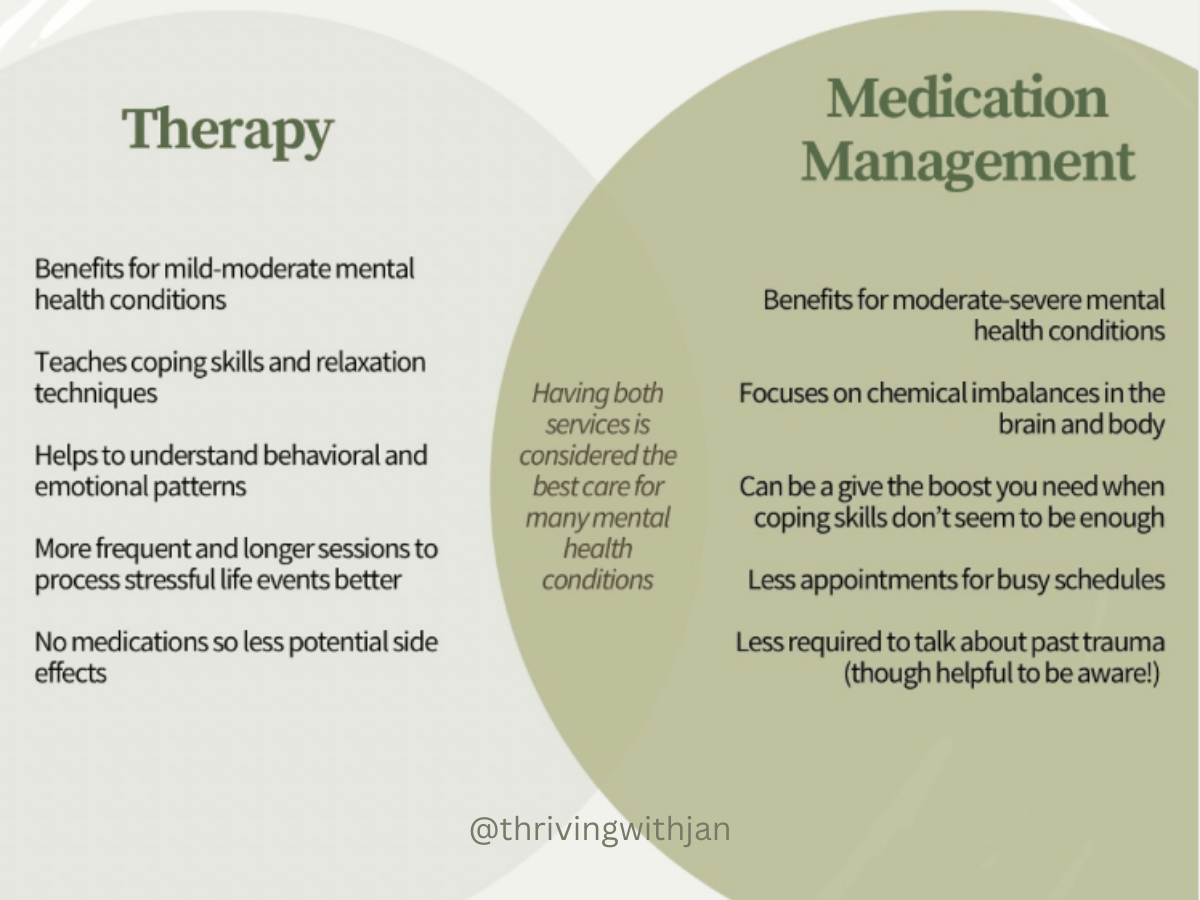
Seeking help from mental health professionals often involves therapy to process what’s happened in the past and develop coping strategies for the present.
But what if we feel like therapy only gets us so far?
A powerful tool to address this stagnancy is by integrating antidepressants or other psychiatric medications to regain a direction towards more positivity and control.
However, it’s common to have some fears that prevent us from exploring this option.
Join me as a I answer common questions and concerns about psychiatric medication management.
The Role of Medication in Mental Health Treatment
Antidepressants are the most commonly prescribed medications for your mental health but mood stabilizers, antipsychotics, or other psychiatric medications may be more appropriate for you depending on your mental health concerns and history.
For the sake of simplicity, I will group all medications in this article by the term “medications” or “antidepressants.”
By addressing the chemical imbalances in your brain, medications can impact various aspects of your wellbeing including the improvement of:
Feelings of anxiety, depression, stress, or anger 😣
An earlier recognition of stress or trauma responses, giving you a chance for timely application of coping mechanisms 🌞
Effectiveness of said coping mechanisms 🏋️♂️
Problems concentration, motivation, sleep, and energy ✨
Let’s address some common concerns about antidepressants and medications
#1: “I don’t want to feel numb!”
We’re adjusting your brain chemistry here, so it’s understandable to have a fear that taking antidepressants, mood stabilizers, or other mental health-related medications might change your personality or make you feel numb.
My goal for my patients is to help them feel more capable of being in control when feelings arise so that you feel more like yourself, not erase your feelings altogether.
#2: “I’m scared of all the side effects.”
Try to remember, these are side effects, not effects. It’s not guaranteed that antidepressants or medications for trauma therapy will cause side effects.
Most side effects are temporary when adjusting to changes as well as manageable in how it shows. If you do experience side effects, you can double check with your provider for guidance. Persisting side effects are usually not a permanent reaction either, as it’s usually reversible by taking away the source that’s causing it.
#3: “I feel anxious about having to talk to a stranger about my trauma.”
When seeing new patients, I usually let them know that the questions I ask are to both get to know your concerns, and where you come from in your mental health journey.
It helps me to understand you better when you answer my questions truthfully, though I have no expectations on how detailed your answers need to be.
On the flip side, some people find that processing trauma is too triggering even with their therapist, and medications can help them be reactive so that they have enough confidence to start facing their past.
#4: “I don’t want to be addicted to medicine.”
Many mental health medications need weeks to adjust properly but most of them, including SSRIs and SNRIs, are non-addictive.
Many providers, including me, do not prescribe medications that have a risk for addiction in consideration of your long-term health.
Ask your provider what their standard of care is on medications.
#5: “What good can medicine do anyways with how my life is going?”
Medications have a lot of potential, but it’s true to say that it’s a normal response to react stressfully to stressful events. That being said, if you are at a point where you feel like your emotions are controlling you more than you’re controlling it, medications support the reverse of that script.
If you feel like you’re not getting the progress you were hoping for in therapy when talking about the problems going on in life, medications can improve your baseline so that you can feel more in capacity to address stressors in your life better.
#6: “I don’t want to take medications for the rest of my life.”
Whether medications should be taken forever or temporarily varies for everyone.
I do urge you to talk to your therapist and provider if you’re interested in trialing a medication taper eventually so that all parties can work together to keep you supported and safe.
Just like glasses for poor vision or insulin for diabetes it’s okay if you need medicine temporarily, and it's okay if you need medicine for life.
What matters most is that you’re receiving treatment that supports the better quality of life that you deserve.
Personalized Treatment Plans for Medication Management and Trauma Therapy
A personalized treatment plan should be, well, personalized.
As a psychiatric nurse practitioner who does medication management for trauma and PTSD, I believe that there is no one-size-fits-all treatment.
Sometimes it’s hard to know what to ask for when seeing a provider so here’s some examples of what you can ask about to advocate for your needs and feel more comfortable with your care.
Clarify expectations.
Some basic understanding points to medications are to know why you’re taking it, what to expect for benefits, what unwanted effects to watch out for, and how long you need to take it to adjust to your body.
Go low & slow.
There’s nothing wrong working with smaller doses or doing smaller adjustments if that helps you feel less anxious about new changes with your medications.
Ask for other options.
At the end of the day, you’re the one who’s taking the medication. It’s important that you feel comfortable with the medication that you take.
If you have certain preferences or concerns about what’s being recommended to you, let your provider know and ask if there are other options.
Ask your provider and therapist to meet.
If you’re unsure whether your provider and therapist are on the same page in treatment goals, you can ask them to touch base with each other. A good provider or clinician shouldn’t be hesitant on collaborating as it helps to support your quality of care.
Take a break.
Sometimes the process of medication management can be overwhelming. Sometimes another appointment to manage feels too much when life gets busy.
It’s okay to hit the pause button or take a break from medication altogether to be able to focus on other areas of your life.
If you want to take a break from medication, consult with your provider. They can help assess safety risks and support your pause.
Medications are not a cure-all…
I always emphasize to my patients that medications are not a cure-all, and this especially is true when it comes to trauma.
As we learned, medications can do a lot, but it can’t make our mind, or our bodies forget what happened to us.
This is why the gold standard of treatment for PTSD and other trauma-related issues are both medications and therapy.
Medications play the role to help improve your baseline and be able to say, “You know what… This isn’t the end of my story. Maybe I don’t have an exact plan right now but I know I can get through this!” whereas therapy helps you really get in the nitty gritty of understanding what happened to us, what are the signs of our past still showing up today, and how can we find internal peace.
Looking to learn more about how medications can help support you and your mental health?
I’d be honored to guide you through this part of your life. Take the first step in reaching out today!
Janelle Aguilon, APN, PMHNP